Rotator Cuff Tears
The shoulder is made up of three bones: the upper arm bone (humerus), the shoulder blade (scapula), and the collarbone (clavicle). The shoulder is a ball-and-socket joint: The ball, or head, of the upper arm bone fits into a shallow socket in the shoulder blade.
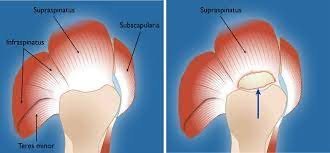
The Rotator cuff is a capsulotendinuos tissue which attaches on the head of the humerus. It is actually the attachment of 4 major muscles that move the shoulder joint, namely , Subscapularis, Supraspinatus,Infraspinatus and Teres Minor The rotator cuff attaches the humerus to the shoulder blade and helps to lift and rotate your arm a rotator cuff tear is a common cause of shoulder pain and disability among adults.
Rotator cuff tears occur in two ways:
- A sudden acute tear may happen when you fall on your arm while it is stretched out. It can also occur when you try to lift something very heavy with a sudden motion.
- A chronic degenerative tear of the rotator cuff tendon occurs gradually over time. This happens more commonly in the elderly people especially when they have a pre existing tendinitis or impingement syndrome. At some point, in time the tendon degenerates and tears suddenly.
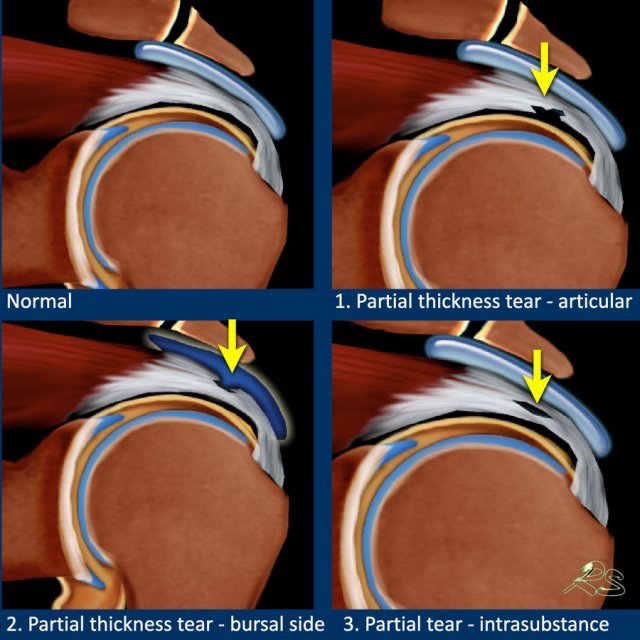
There are two types of rotator cuff tears:
- Partial cuff teras: are those in which some fibres of the cuff are still attached to the humeral head. These might heal without surgery
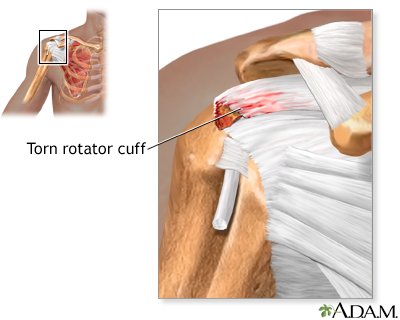
- complete, full thickness tears: are those in which the tendon is ripped off the humeral head completely . It may be as small as a pinpoint, or the tear may involve the entire tendon. These tears need surgical repair.

Symptoms
There is excruciating pain when the rotator cuff tears after a fall or trauma. You may also feel or hear the tissue tearing.Immediately after the injury, you will experience difficulty in lifting the shoulder and arm. It may be hard to move your shoulder or raise your arm above the shoulder.
With a chronic tear, you often do not notice when it began. This is because symptoms of pain, weakness, and loss of motion worsen gradually over time.
Rotator cuff tears often cause night pain . Sleeping on affected side is difficult.. The pain may even awaken you leading to sleep disturbances. During the day, the pain is more tolerable, and usually only hurts while doing overhead activity or doing rotational movements Over time, the symptoms get more severe, and are not relieved by conservative measures like medicines, rest, or exercise.
Diagnosis
Dr Ahmed will do some clinical tests during the consultation as rotator cuff tears are easily diagnosed on clinical examination.
- Drop Arm test
- Empty Can / Full Can test
- Bear Hug Test
- Lift off test
Above are some tests that will be performed for the diagnosis
Xray
Although rotator cuff tissue is not seen on Xray , Xrays are done routinely to assess the status of the shoulder joint and bones that form it.
MRI
This is the gold standard to diagnose rotator cuff tears.
A good MRI can describe the geometry of the tear , its extent, the amount of retraction and also about other associated pathologies like subacromial bursitis, acromion morphology, fatty infiltration of the cuff , cartilage status, etc
Treatment
Complete Rotator cuff tears do not heal on their own without surgery, but many patients can improve functionally and decrease pain with nonsurgical treatment by strengthening their shoulder muscles. Just because there is a tear, does not mean a surgery is always needed.
Approximately 8 out of 10 people with partial tears get better with nonsurgical treatments, but it can take up to a year for the condition to improve.
Nonsurgical treatments include:
- Activity modification: to change or stop doing activities that cause pain. This allows rest to the shoulder.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to minimize pain and swelling
- Opioids: if long term therapy is required
- Physical therapy to strengthen the shoulder girdle muscles
- Steroid injections to ease pain and swelling.
Surgical Treatment
Dr Ahmed may recommend surgery if you have a complete tear or nonsurgical treatments don’t help in cases of partial tears.
Most rotator cuff surgeries are done arthroscopically through keyhole incisions. The can be done on a day care basis, ie. Patients go home the same day, but the overall recovery after this surgery is very substantial and can take up to a year or more.
Some tears are not repairable due to the size and/or age of the tear, and may require reverse shoulder replacement, tendon transfer, Superior Capsule Reconstruction (SCR)or a debridement of scar tissue without repair. During surgery, Dr Ahmed would
- Insert an arthroscope (small camera) through a tiny incision in your shoulder.
- Confirm the diagnosis with the camera
- Look for any other injuries
- Asses the rotator cuff tear pattern and reducibility
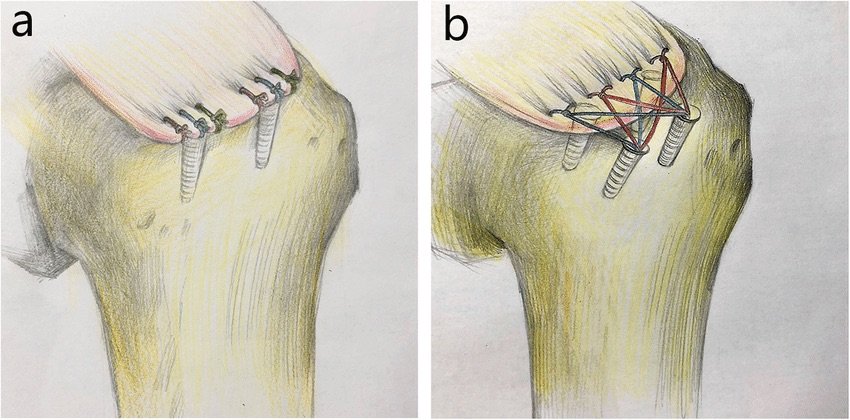
- Inserts tiny instruments into small incisions in your shoulder to remove inflamed bursa(subacromial decompression + Bursectomy) bone spurs(Acromioplasty) and repair the torn rotator cuff tendon to the humeral head greater tuberosity footprint
For a partial tear, Dr Ahmed may only need to trim the frayed edges of a partially torn tendon. This is called debridement procedure and it keeps the torn edges of the tendon from impinging in the joint and further tearing more. After surgery, you would be advised to wear a shoulder immobiliser to immobilize your shoulder for four to six weeks. Physical therapy is advised after that . Most people regain shoulder function and strength within four to six months after surgery, but full recovery may take up to 12 months in some patients.
Frequently Asked Questions(FAQ's)
A rotator cuff tear involves damage to one or more of the four tendons that stabilize the shoulder joint: supraspinatus, infraspinatus, subscapularis, and teres minor. Tears can be acute (sudden injury) or chronic (degenerative over time).
Diagnosis involves:
Clinical examination: tests like the Drop Arm, Empty Can, Bear Hug, and Lift-Off tests.
Imaging: X-rays to rule out bone issues; MRI or ultrasound to assess soft tissue damage.
Surgical options include:
Arthroscopic repair: minimally invasive procedure to reattach the tendon to the bone.
Open surgery: used for larger or more complex tears.
The choice depends on tear size, location, and patient activity level.
Rotator cuff tears can be treated surgically using arthroscopic repair, which is minimally invasive and involves small incisions to reattach the tendon, or open surgery for larger or complex tears. In some cases, a mini-open repair or tendon transfer may be recommended depending on the tear size and tissue quality.
Not always. Arthroscopic or minimally invasive surgery is ideal for small to medium tears and patients with good tendon quality. Large, chronic, or complex tears with significant tissue loss may require open or combined approaches for better repair and long-term stability.
Doctors consider factors like tear size, location, tissue quality, patient age, activity level, and overall health. Imaging studies such as MRI or ultrasound help assess the damage, allowing the surgeon to choose the most effective approach—arthroscopic, open, or mini-open—to restore shoulder function safely.